Have you ever walked into a room and completely forgotten why you went there? Or struggled to remember a conversation from yesterday? People forget things sometimes. But for those with depression, memory lapses happen more often. This can be frustrating. Depression and memory loss are linked, impacting millions. Many people don’t know that their memory issues come from their mental health.
Can depression cause memory loss? Yes, depression impacts memory and thinking. It changes the brain. It causes neurotransmitter imbalances and raises stress hormones. About 85% of people with depression have trouble with memory or concentration. The encouraging news? Memory problems related to depression often improve with appropriate treatment for the depression. Our complete guide to depression provides a comprehensive context.
Medical Disclaimer: This article provides educational information about depression and cognitive function. It is not a substitute for professional medical diagnosis or treatment. If you experience memory problems or depression symptoms, consult qualified healthcare professionals.
How Depression Affects Your Brain
Your brain is always making new memories. It also finds old ones and processes what’s around you. When depression develops, this intricate system faces significant disruption. Imagine your brain as a busy office. When things run smoothly, tasks get done quickly. Depression is like half the team calling in sick—the rest struggle with more work.
Depression can lead to memory loss, especially when we look at brain changes. The hippocampus is a seahorse-shaped part of your brain. It helps you form and retrieve memories. Neuroimaging studies show that the hippocampus often shrinks in people with depression. This is especially true for those with chronic, untreated depression. This change isn’t permanent. Research shows the hippocampus can heal with treatment. This explains many memory issues.
The prefrontal cortex controls executive functions such as decision-making and working memory. During depression, this area shows less activity. This reduced function makes multitasking feel impossible and concentration exhausting. The amygdala is your emotional center. It becomes hyperactive, which boosts your emotional responses. This can also hurt your ability to form neutral memories. You often remember upsetting events well, but positive or neutral ones can be tough to recall.
Chemical messengers called neurotransmitters also play critical roles. Serotonin supports cognitive functions, including memory consolidation. Depression causes serotonin deficiency, directly impacting memory formation and retrieval. Dopamine helps with motivation and working memory. When dopamine levels drop, even simple tasks can feel hard to remember. Norepinephrine influences attention, and its dysregulation impairs sustained attention necessary for memory formation.
Chronic depression elevates cortisol, your primary stress hormone. Cortisol can be helpful in short bursts. But if it stays high for too long, it can hurt hippocampal neurons. This also stops neurogenesis, which is the creation of new brain cells vital for memory. Severe depression can lead to memory loss. Studies show this happens partly because of cortisol's harmful effects on brain structures. This creates a damaging cycle.
What Memory Loss Feels Like Daily
Can depression cause short-term memory loss? It's not possible to remove the adverb. Working memory is like your brain's notepad for holding information temporarily. It can get disrupted more easily. You may forget what you read, lose focus during talks, or enter rooms without remembering why. These aren't signs of dementia. Depression drains mental resources. Your brain usually saves these for memory.
Can depression cause long-term memory loss affecting past events? People often struggle to recall recent conversations, appointments, or activities. Distant memories, like childhood moments and big life events, frequently stay clear in our minds. This pattern differs dramatically from dementia, where older memories usually fade first.
The cognitive fog feels like thinking through molasses. Everything takes longer. Processing information becomes exhausting. Tasks requiring mental speed feel impossible. Neuropsychological tests show that people with depression have slower processing speeds. This affects all areas of thinking.
Can anxiety and depression cause memory loss together? When these conditions co-occur, memory problems often intensify. Anxiety adds physiological arousal and worry to depression's cognitive burden. Understanding stress and anxiety shows how they affect our thoughts.
Why This Happens
Understanding how depression causes memory loss requires examining multiple mechanisms. Chronic inflammation linked to depression releases cytokines. These cytokines cross the blood-brain barrier. They interfere with neurotransmitter function and harm neurons, especially in the hippocampus.
Your brain's ability to form new neural connections—neuroplasticity—decreases during depression. Brain-derived neurotrophic factor (BDNF) is vital for neuroplasticity and memory. It reduces significantly during depressive episodes. Antidepressant treatments often work partly by increasing BDNF levels.
Psychological factors play major roles, too. Negative thought cycles characteristic of depression consume enormous cognitive resources. Rumination—repetitive negative thinking—hijacks your attention system. When your mind keeps replaying worries, it has less space for making new memories or finding old ones.
Can untreated depression cause memory loss that worsens over time? Longitudinal studies say yes. Chronic, untreated depression leads to worsening cognitive decline. Memory issues get worse the longer depression lasts. This highlights why early intervention matters.
Depression or Dementia? Critical Differences
Can depression cause memory loss instead of a progressive neurological disease? Distinguishing these conditions proves crucial, especially for older adults. Depression-related memory problems typically involve poor concentration affecting memory encoding. Dementia involves actual memory storage and retrieval deficits.
People with depression often respond with "I don't know" when asked questions. This shows they may struggle with concentration. Those with dementia frequently confabulate—making up answers—because they genuinely don't remember. Depression-related memory problems fluctuate with mood. Dementia progresses steadily regardless of emotional state.
The good news is that memory loss from depression often gets better with treatment. In contrast, dementia-related decline gets worse over time. Cognitive testing patterns differ, too. Depression shows subcortical patterns with slowed processing. Dementia shows cortical patterns with true amnesia and language difficulties. Understanding early signs of mental health issues supports recognizing when evaluation becomes necessary.
Recognizing the Signs
Can depression cause confusion and memory loss in daily life?
Signs include:
- Forgetting recent conversations.
- Difficulty following complex instructions.
- Frequently losing items.
- Struggling to concentrate.
- Experiencing mental fog.
These lapses accumulate over time, becoming plain through their impact on routine activities.
The mental fog feels like thinking through a thick cloud. Decisions that should be simple become overwhelming. This affects work productivity, relationships, and learning. Can depression cause memory loss in elderly individuals more severely? Age-related factors may compound depression's effects, though depression remains treatable at any age.
Who's at Risk
Can severe depression cause more memory loss than milder forms? Yes—greater severity correlates with worse cognitive impairment. Can long-term depression cause memory loss that's harder to reverse? Duration matters. Chronic depression shows stronger cognitive effects than brief episodes.
Can postpartum depression cause memory loss in new mothers? Hormonal changes, lack of sleep, and depression can greatly affect memory. Can stress and depression cause memory loss together? The synergistic effect substantially impairs memory beyond either factor alone.
Can depression medication cause memory loss? Some medications can affect memory for a short time. But treating depression usually boosts brain function. Healthcare providers can adjust medications if problems persist.
Getting a Proper Diagnosis
Diagnosing cognitive impairment from depression requires careful evaluation. This includes:
- Psychiatric assessment
- Cognitive testing
- Medical evaluation
- Neuropsychological testing is used if the diagnosis is unclear.
Do not include thyroid disorders, vitamin deficiencies, sleep disorders, medication effects, or early dementia in the evaluation. Understanding psychiatric disorders shows us how mental health issues affect our thoughts.
Treatment Approaches
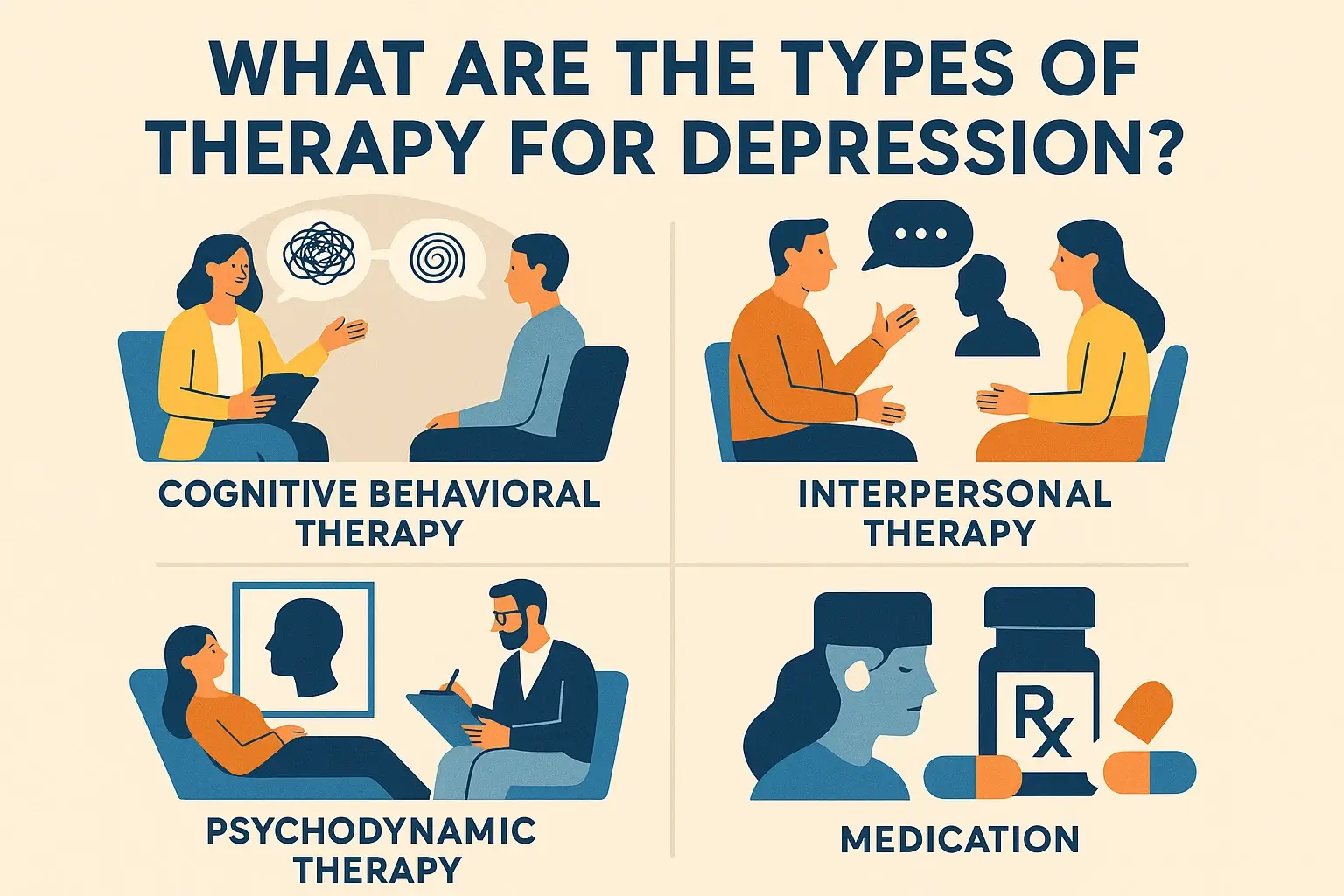
Types of therapy for depression effectively address both mood and cognitive symptoms. Cognitive Behavioral Therapy (CBT) helps spot and change negative thoughts. These thoughts can drain mental energy. Cognitive remediation therapy specifically targets memory and attention problems.
Can anti-depression pills cause memory loss or help with it? Modern antidepressants typically improve cognitive function by treating underlying depression. Clinical studies show that effective antidepressant treatment helps 60-70% of people with memory problems. Can antidepressants improve memory? Yes, primarily by treating depression.
Lifestyle interventions provide powerful support. Sleep optimization proves crucial. Regular physical exercise increases BDNF, promoting neuroplasticity. Stress management techniques, including mindfulness meditation, have proven to deliver measurable improvements. Nutrition supporting brain health may complement other treatments.
Recovery Timeline
How long until memory improves? Most people notice initial cognitive improvements within 4-8 weeks of effective depression treatment. Concentration and attention often first enhance. Memory encoding and retrieval will improve, but full cognitive recovery may take months.
Will my brain go back to normal after depression? Research provides hopeful answers. Substantial cognitive recovery occurs with successful treatment. Brain imaging studies show hippocampal volume often increases following depression treatment. Most people regain baseline cognitive function. Some studies show that small deficits can linger after many depressive episodes. This highlights the need to keep up treatment and prevent relapse.
Prevention and Long-Term Health
Early depression treatment minimizes cognitive impact. Recognizing symptoms promptly and seeking treatment protects both mood and cognitive function.
You can boost your cognitive reserve by:
- Engaging in education
- Doing stimulating activities
- Socializing
- Exercising
These efforts may help protect against the cognitive effects of depression.
Mental health awareness supports recognizing problems early. Regular mental health check-ups help catch depression recurrences. Keeping up with treatment during recovery helps stop relapse. This protects the brain from the cognitive effects of depression.
Conclusion
Understanding that depression can cause memory loss and confusion encourages people to seek help. This way, they don’t need to fear dementia. The reversible nature of depression-related cognitive impairment offers genuine hope. These aren't permanent deficits—they're symptoms of a treatable medical condition.
If you have memory problems and depression, remember these symptoms are treatable. They do not reflect personal failings. Professional evaluation distinguishes depression from other causes while guiding effective treatment. With appropriate care, both your mood and memory can show considerable improvement. Treatment works. Recovery is possible. Your future can include both a better mood and clearer thinking.


Comments