Bipolar disorder and depression can be confusing. They share many symptoms, which makes it hard to tell them apart. Both involve periods of deep sadness, loss of energy, and difficulty finding joy in life. Finding the unique traits of each condition is key. This helps in choosing the right treatment and support.
Why This Comparison Matters
Many people struggle with how similar depression appears in both situations. When someone has their first depressive episode, doctors can’t always tell if it’s major depressive disorder or the start of bipolar disorder. The key difference shows up when we look at the pattern of mood changes over time.
About 21 million adults in the U.S. have major depressive disorder. Also, around 4.4 percent will face bipolar disorder at some point in their lives. These numbers show how common both conditions are. Understanding their differences helps many people and families.
Educational Purpose and Scope
This resource compares major depressive disorder and bipolar disorder. It helps people understand these mental health conditions better. At Gendrics, we aim to help people understand complex mental health topics. We provide clear, accessible education. This empowers better conversations with healthcare providers.
But, this information serves educational purposes only. Only qualified healthcare professionals should handle diagnosis and treatment planning. They can assess your full history, symptoms, and personal situation. Don't try to diagnose yourself or others from information. A professional evaluation looks at many factors that an article can't cover.
Clinical Definitions: What Are These Conditions?
Understanding what doctors mean by major depressive disorder and bipolar disorder shows us how these conditions are different.
Major Depressive Disorder Explained
Major depressive disorder, or MDD, is also known as clinical depression. It means having one or more major depressive episodes. People with MDD do not have manic, hypomanic, or mixed episodes. A major depressive episode is when you feel sad or lose interest in things you usually enjoy. This lasts for a significant part of the day, on almost every day, for a minimum of two weeks. You also have several other symptoms.
People with major depression go through low periods. These can last weeks, months, or even years if not treated. Some people go back to their normal mood and routine between episodes. Others keep feeling milder symptoms. Bipolar disorder and clinical depression mainly differ in one key way: major depression doesn’t have the extreme highs seen in bipolar disorder.
Bipolar Disorder Explained
Bipolar disorder is a type of mood disorder. It causes mood swings. You can feel very low, like in deep depression, or very high, known as mania or hypomania. The name bipolar refers to these two opposite poles of mood. This condition isn’t about regular mood changes. It causes dramatic shifts that can significantly impact daily life and relationships.
Bipolar I disorder involves at least one manic episode. This episode lasts at least one week or requires hospitalization. People with Bipolar I can have depressive episodes. However, these episodes aren't required for the diagnosis.
Bipolar II disorder involves at least one hypomanic episode and one major depressive episode. Hypomania is a milder type of mania. It doesn't cause as much trouble or need hospitalization.
Understanding bipolar and unipolar depression is important. Unipolar refers to major depression, which only includes the depressive side. Bipolar, on the other hand, consists of both depressive and manic moods.
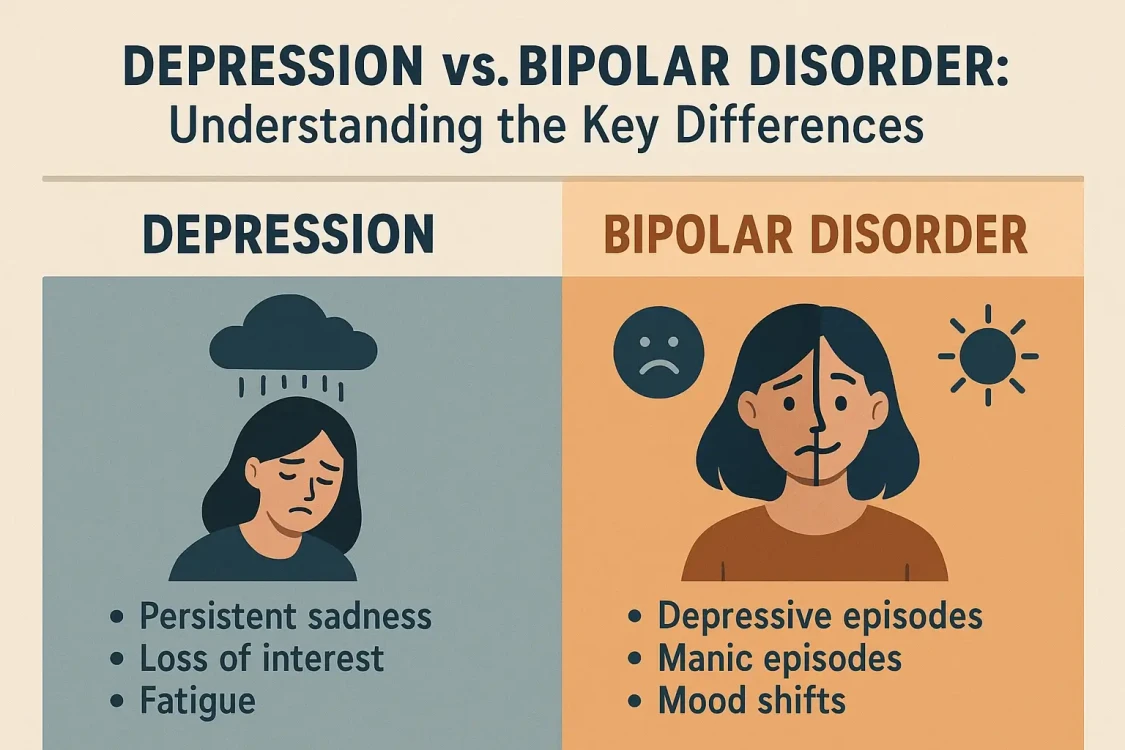
Symptom Comparison: Overlap and Distinctions
To spot bipolar and depression symptoms, understand their similarities during depressive episodes. You also need to understand the key differences that set them apart.
The Depressive Phase: Shared Symptoms
Major depressive disorder and depressive episodes in bipolar disorder can appear quite alike. During depression, people may feel sad, anxious, or empty for a long time. They might lose interest in activities they once enjoyed. Changes in appetite can lead to weight loss or gain.
Sleep issues can cause them to sleep too much or too little. They may feel exhausted even after resting. Feelings of worthlessness or guilt can also occur. It may become difficult to think with clarity, focus, or make decisions. Some may even have thoughts of death or suicide.
Misdiagnosing bipolar disorder as depression happens often. These similarities help explain why. When someone seeks help for depression, their symptoms may seem like major depression. But a doctor needs to ask specific questions about past mood patterns to tell the difference.
The Defining Feature: Mania and Hypomania
Doctors mainly diagnose bipolar disorder versus depression based on manic or hypomanic episodes. Their presence or absence is key. Knowing about elevated moods can help you tell if it’s bipolar disorder or depression.
Mania in Bipolar I disorder lasts at least one week. During this time, high energy, expansiveness, or irritability mark the mood. People also show increased energy and activity. During mania, people may feel unstoppable, on top of the world, or very irritated and restless. This isn't a good feeling—it's a mood state that can cause big problems in daily life.
Common features of mania include:
- Believing you possess unique skills or having an inflated sense of confidence.
- Needing less sleep but not feeling tired.
- Talking a lot more or feeling a constant urge to talk.
- Having racing thoughts that are hard to manage.
- Being distracted by minor things.
- Significantly increasing goal-directed activities or experiencing restlessness.
- Taking risks, such as spending sprees, reckless driving, or impulsive decisions.
Hypomania in Bipolar II disorder shows similar symptoms but is less severe. It lasts for at least four days. During hypomania, people often feel productive, creative, and energetic. They may not see anything wrong. Hypomania often feels good, especially when compared to depression. However, others usually notice changes in behavior, mood, and activity levels.
Understanding mood swings in bipolar disorder and depression shows key differences. In major depression, mood changes vary in severity. In bipolar disorder, mood swings shift between depression and mania or hypomania.
Recognizing the Pattern Differences
The pattern of mood episodes over time provides crucial information for diagnosis. In major depression, mood stays in the depressive range, though severity might vary. Some people have mood episodes that come and go. Others deal with ongoing depression that doesn't fade.
In bipolar disorder, people experience both depressive episodes and manic or hypomanic ones. These episodes can follow a regular pattern. They may also occur without pattern or have periods of normal mood in between. Some people experience rapid cycling with four or more mood episodes in a year.
Signs of bipolar disorder versus depression include:
- Mood episodes with both highs and lows.
- Sudden increases in energy and less need for sleep.
- Behavior changes that seem out of character or lead to issues.
How Professionals Differentiate Conditions
Doctors distinguish between bipolar disorder and depression through careful evaluation. This process is crucial for accurate diagnosis. It leads to the right diagnosis and proper treatment.
The Key Diagnostic Differentiator
The main difference between major depressive disorder and bipolar disorder is the presence of manic or hypomanic episodes, either now or in the past. A doctor diagnoses bipolar disorder when a person has experienced mania or hypomania. This is true even if their depressive episodes happen more often or are more intense.
This distinction matters greatly because treatment approaches vary widely. Using the wrong treatment can worsen symptoms or create new problems, making an accurate diagnosis essential for effective care.
Comprehensive Assessment Methods
Diagnosis typically involves a thorough evaluation by a qualified mental health professional. This assessment includes a comprehensive clinical interview. It covers current symptoms, when they began, how long they've lasted, and their impact on daily life. The interview looks at your psychiatric history. It includes past mood episodes, treatments you tried, and how you responded to them.
Family psychiatric history is key. Depression and bipolar disorder often run in families. Knowing if close relatives have mood disorders helps doctors assess your risk and symptoms.
Mental health experts follow guidelines from the Diagnostic and Statistical Manual of Mental Disorders. This helps them make consistent and accurate diagnoses. These criteria outline the required symptoms, their duration, and the level of impairment for each diagnosis.
Tools for Tracking Patterns
Mood charts or daily logs track patterns over time. They provide important information to help distinguish between different conditions. Tracking your mood, energy, sleep, and activities shows patterns you may not remember.
Bipolar screening and depression tests ask about past manic and hypomanic symptoms. Standard depression screening tools often miss these questions. This is one reason why misdiagnoses occur.
Some people wonder if depression can turn into bipolar disorder. The condition doesn’t change from one to the other. A doctor might first diagnose a person with depression based on early episodes. The bipolar diagnosis usually becomes clear later. This happens after symptoms of mania or hypomania appear.
Why Accurate Diagnosis Matters
The accuracy of diagnosing these conditions is key. Treatment methods differ a lot. Taking antidepressants alone for bipolar depression can lead to manic episodes. It may also cause rapid mood cycling, which can worsen the condition. Mood stabilizers used for bipolar disorder are generally unnecessary for major depression.
Knowing if you have bipolar disorder or major depression is important. It helps you spot warning signs, create coping strategies, and set realistic treatment goals.
General Management Strategies
Understanding treatment for bipolar disorder and depression shows key differences in management. Both conditions involve a mix of professional care and self-care strategies.
Management of Major Depressive Disorder
Treatment for major depression usually begins with psychotherapy, medication, or both. This choice depends on how severe the symptoms are and what the individual prefers. Evidence-based therapies, such as Cognitive Behavioral Therapy (CBT), help you spot and change negative thoughts. These thoughts often cause depression. Interpersonal Therapy works on improving relationships and communication skills.
Bipolar disorder medication is very different from depression treatment during the depressive phase. For major depression, antidepressant medications serve as the primary treatment.
Common types are:
- SSRIs: fluoxetine, sertraline
- SNRIs: venlafaxine, duloxetine
Other classes vary based on individual responses and side effects.
Many people with major depression find that Therapy and medication work well together. This combo tackles the biology of depression. It also looks at thought and behavior patterns that make it worse. Regular exercise, better sleep, and stress management can help support professional treatment. They provide extra relief from symptoms.
Recovery from bipolar disorder vs depression follows different timelines and patterns. In major depression, many people notice improvement within weeks or months after starting treatment. Full recovery is possible for many. But some may face recurring episodes that need ongoing care.
Management of Bipolar Disorder
Bipolar disorder treatment mainly uses mood stabilizers and certain antipsychotic medications. These are the key approaches. These medications prevent both manic and depressive episodes. They provide stability that antidepressants alone cannot offer.
Common mood stabilizers are:
- Lithium: This has the longest history of stopping mood episodes.
- Valproic acid: This often helps those with rapid cycling.
- Lamotrigine: This is especially good at preventing depressive episodes.
Antipsychotic meds like quetiapine, olanzapine, and aripiprazole help stabilize mood. They also treat acute episodes.
Antidepressants and bipolar disorder need careful consideration. Antidepressants can trigger manic episodes or rapid cycling in people with bipolar disorder. Antidepressants, when used, usually work with mood stabilizers. This helps reduce risks. Many psychiatrists skip antidepressants for bipolar depression. They prefer mood stabilizers and antipsychotics instead.
Therapy for bipolar disorder and depression uses different methods. These approaches target the specific challenges of bipolar disorder. Psychoeducation helps people grasp their condition. It teaches them to spot early warning signs of mood episodes. It also highlights the importance of sticking to their medication.
Cognitive Behavioral Therapy for bipolar disorder teaches ways to manage mood swings. It also helps deal with the effects of past manic episodes. Family-focused Therapy helps families understand the condition. It also teaches them how to support their loved ones. At the same time, it shows ways to keep healthy boundaries.
Lifestyle and Natural Management
Managing bipolar disorder and depression with lifestyle changes can boost professional treatment. However, these methods work best when combined with, not as a replacement for, medical care.
Lifestyle changes for bipolar disorder and depression include keeping regular sleep schedules. Sleep problems are key to bipolar disorder. They can spark manic episodes. Regular exercise helps both conditions. It boosts mood, lowers stress, and supports health. Stress management through meditation, yoga, or relaxation techniques helps prevent episode triggers.
Avoiding alcohol and recreational drugs is important for bipolar disorder. These substances can trigger episodes and make medications less effective. For major depression, substance use often worsens symptoms and reduces treatment effectiveness.
Coping strategies for bipolar disorder vs. depression differ in important ways. People with major depression can improve through behavioral activation. This approach enhances their activities and social interactions over time. For bipolar disorder, coping strategies aim to maintain stability. They help with spotting early warning signs of episodes. Also, having action plans is key to managing symptoms before they get worse.
Support Systems and Resources
Support for those with bipolar disorder or depression includes:
- Professional treatment teams.
- Understanding family and friends.
- Support groups for sharing experiences and strategies.
- Community mental health resources for ongoing care and crisis support.
Both conditions need strong support systems. However, the type of support may vary. Bipolar disorder needs families to help spot early warning signs. They help ensure that individuals follow treatment, especially if they lack insight. Major depression support usually emphasizes encouragement and companionship during tough times. It also offers gentle help with daily tasks that can feel overwhelming.
Understanding how these conditions affect daily life is important. Even though they are different, both have a strong impact. Luckily, with the right treatment and support, they can be managed well.
Daily Life Challenges
Both conditions affect work, school, and daily responsibilities, though in different ways. Major depression causes constant fatigue, trouble focusing, and low motivation. This makes even simple tasks seem hard. Bipolar disorder leads to challenges during depressive episodes. It also brings problems during manic or hypomanic periods. In tough times, people may not think clearly. This can lead to choices that have consequences.
Both conditions affect relationships. Depression can lead you to pull away from loved ones. It may make it hard to show affection. You might also find it tough to join in social activities. Bipolar disorder impacts relationships in several ways. During manic episodes, behaviors can be erratic. In depressive episodes, there is often a strong need for support. Plus, managing this ongoing condition requires consistent treatment, which can be challenging.
Addressing Common Misconceptions
Many people ask if bipolar disorder is worse than depression. However, there’s no easy answer. Both conditions cause significant suffering and impairment. Bipolar disorder needs more complex treatment and managing manic episodes. Major depression can also be severe, chronic, and life-threatening. Neither condition is worse - they're different challenges requiring different approaches.
Another common question is whether bipolar disorder and depression are the same thing. While they share depressive symptoms, they're distinct conditions. Bipolar disorder has manic or hypomanic episodes, while major depression does not. This key difference affects how we treat and manage the condition over time.
Understanding bipolar and depression comorbidity is important. Some people have both conditions. They may have bipolar disorder. They could also face extra depressive episodes that don't follow the usual pattern. This comorbidity requires comprehensive treatment addressing both conditions.
Hope and Recovery
Both major depression and bipolar disorder are treatable conditions. Many people feel much better with the right professional treatment. However, it may take time to find the best approach.
Recovery doesn't necessarily mean never experiencing symptoms again. For many, it means managing symptoms well. This helps reduce how often episodes happen and how severe they are. It also supports good functioning at work and in relationships. It's about living a meaningful and fulfilling life, even with a mental health condition.
The journey with either condition often includes setbacks alongside progress. The key is to stay connected with treatment providers. Use coping strategies regularly. Keep your support systems strong. Don't give up when challenges arise.
Perspective on Mental Health Education
At Gendrics, knowing about mental health helps you speak up for yourself. It also enables you to work better with healthcare providers. Our mission is to give clear, accurate information. This allows people to see when they need help and what types of help are best for them.
Our Educational Approach
We compare depression and bipolar disorder to highlight our commitment to mental health. Understanding these differences helps people talk better with healthcare providers. It also aids in grasping personal experiences or those of loved ones.
Our depression resources explore major depressive disorder. We cover symptoms, treatments, and coping strategies. The psychiatric disorders section includes information on bipolar disorder and other mood disturbances. This helps readers see the full range of mood disorders.
We stress that mental health education should support, not replace, professional care. Information helps you ask good questions. It enables you to spot symptoms that need evaluation and engage in treatment decisions. However, diagnosis and treatment planning need professional expertise that considers your entire situation.
Connecting to Comprehensive Care
To know if you have bipolar disorder or depression, start by recognizing symptoms. Then, seek a professional evaluation. If you see signs in yourself or someone else, it’s important to reach out to a mental health professional.
These professionals can assess your situation, give an accurate diagnosis, and suggest treatments. They can also adjust plans based on your response and needs. This personalized approach is more effective than self-diagnosis or self-treatment. Mental health conditions can differ greatly, even among those with the same diagnosis.
Conclusion
Bipolar disorder includes depression, but it also has manic or hypomanic episodes. Major depressive disorder focuses only on depression. This key difference changes how we understand, diagnose, and treat these conditions.
Knowing the difference between bipolar disorder and depression is crucial for accurate diagnosis. An incorrect treatment can be harmful or ineffective. In contrast, the right treatment can greatly improve symptoms and quality of life.
This information aims to educate and enhance understanding of these conditions. If you see symptoms in yourself or someone nearby, talk to a qualified medical or mental health professional. Both conditions can be treated. With the right diagnosis, effective treatment, and recovery follow.
At Gendrics, we dedicate ourselves to supporting your mental health journey. We provide education, awareness, and reliable information on emotional wellness. Check out our resources on depression, bipolar disorder, and other mental health topics. They can help you understand these issues better.


Comments